60 years old female with AKI on CKD
11/05/2021
Intern: Hema Pushpika
PG- I: Sai Charan
PG-II: A.Vaishnavi
Faculty on call : Dr. Vijaya lakshmi
This is an online e log book to discuss our patient de-identified health data identified health data shared after taking his/her/guardians signed informed consent.
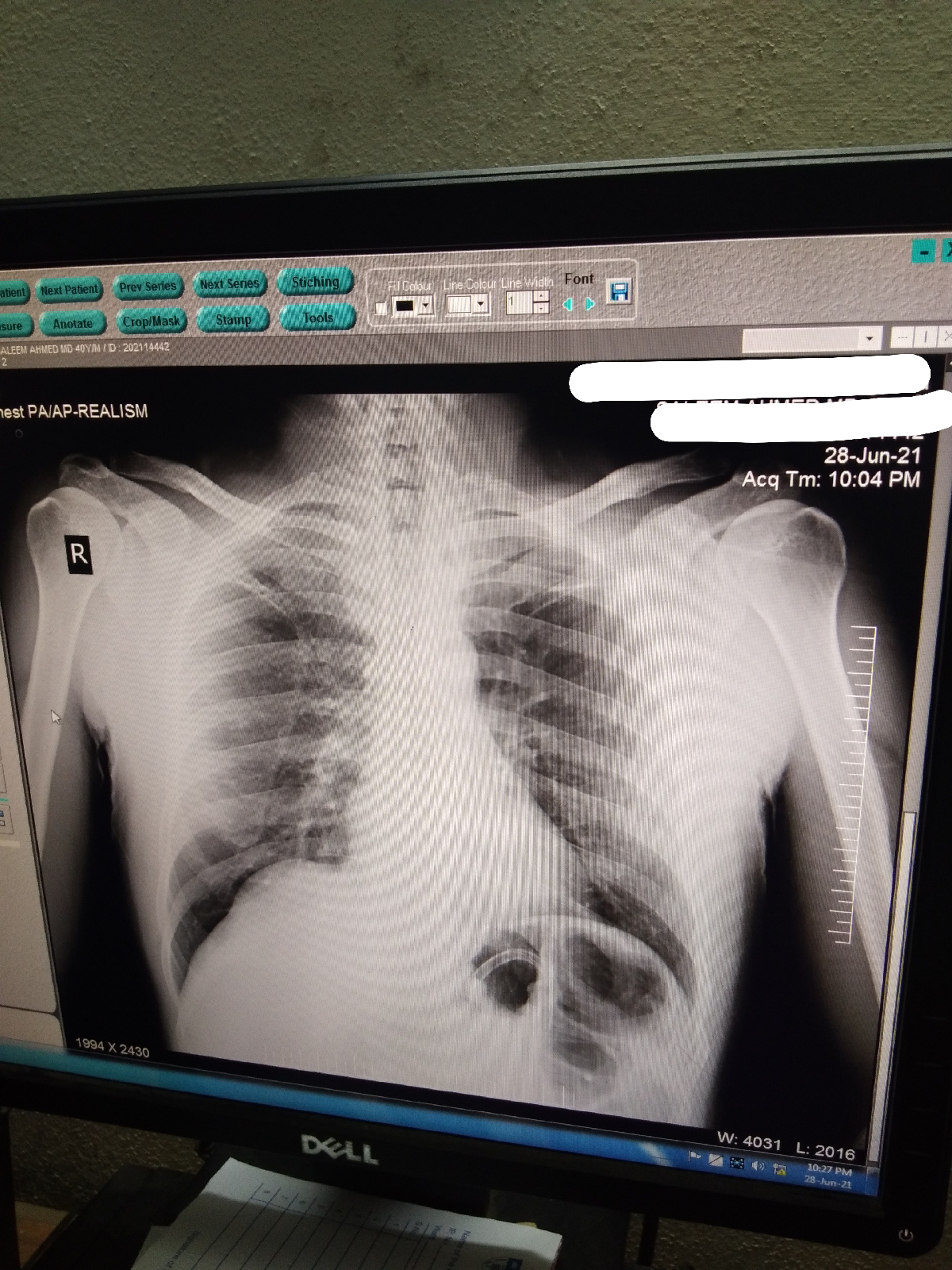
INVESTIGATIONS:
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 60 year old female came with c/o pain abdomen in left loin region since 10 days
Decreased urine output since 10 days
Burning micturition since 10 days
h/o one episode fever 10 days back which is low grade and 2 episodes of vomiting for 2 days
Patient was apparently normal 20 years back , then she developed pain abdomen , decreased urine output then she was told that her right kidney was failed and she need to undergo nephrectomy if not her left kidney will be effected . Because of which she underwent nephrectomy 20 years back.
later she had suprapubic pain with burning sensation 7 years back and was told that she had a wonderful on cervix for which she underwent hysterectomy.
6 years back she had similar complaints for which conservative management was done
K/c/o Hypertension since 5 years and on medication
Not a k/c/o DM/TB/BA
H/o decreased appetite since 10 days
On Examination:
Patient was conscious, coherent and cooperative
No signs of cyanosis, clubbing, lymphadenopathy
Temperature: afebrile
Pulse rate : 86 bpm
Respiratory: 16 cpm
BP : 150/90 mm Hg
Spo2: 96% at room air
GRBS: 160 mg/dl
Systemic examination:
CVS: S1,S2 HEARD
RS: BAE present
CNS: NFND
P/A:
INSPECTION:
Shape - obese
umbilicus- shape inverted , no herniations, no discharges
Movements on respiration - normal
Skin over abdomen is smooth and no pigmentation
no engorged veins, no visible pulsations
PALPATION:
Inspectory findings are conformed on palpation
Abdomen is soft
Non tender
No organomegaly
No palpable masses
Auscultation : bowel sounds are heard
Tunnel obesity:
TREATMENT:
IVF 1 unit of NS @ UO + 30 ML/HR
INJ. LASIX 40 mg iv/bd IF SBP > 110 mmHg
vitals monitoring
strict i/o charting
temperature monitoring
















Comments
Post a Comment