A 28 year old male with quadreparesis secondary to infectious spondylitis
This is an online e log book to discuss our patient de-identified health data identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 28 year old male came with chief complaints of sudden fall followed by weakness of both the lower limbs and loss of hand grip 10 days back, associated with bowel and bladder incontinence.
Patient was apparently asymptomatic 1 month back, following which he developed productive cough, low grade fever for which he underwent sputum studies and tested positive for AFB bacilli and started ATT - HRZE regimen, 2 tab according to weight/PO/OD.
He developed generalized weakness and myalgia 15 days back.
10 days back, patient got up from bed and went to open the door and suddenly fell down, with no loss of consciousness . Following which his brother got him up and since then Patient developed bowel and bladder incontinence.
No h/o sensory impairment.
He is a known case of TB since 1month and on medication ATT - HRZE
Not a known case of DM,HTN, ASTHMA, EPILEPSY, THYROID DISORDERS, STROKE, CAD.
Personal history:
Diet - mixed
Appetite - normal
Sleep - Adequate
Bowel and bladder incontinence + since 1 week
No allergies
No addictions
Family history:
His father is a known case of TB and used ATT for 2 years
On Examination:
Patient is conscious, coherent, co-operative and oriented to time, place and person
No pallor, icterus, cyanosis, clubbing, koilonychia, lymphadenopathy and edema.
Temperature - afebrile
PR - 80 BPM
RR - 16 cpm
BP - 100/70 mm Hg
CNS:
Speech - normal
No signs of meningeal irritation
Right. Left
Tone: UL. N. N
LL increased Increased
Power UL. 4/5. 4/5
LL. 1/5. 1/5
Cranial.nerves. : Intact
Sensory system : normal
Reflexes:
Right. Left
Biceps. 3+. 3+
Triceps. 3+. 3+
Supinator. 2+. 2+
Knee. 3+. 3+
Ankle. 3+. 3+
Plantar: extensor
CVS:
S1, S2 heard
No thrills
No Murmurs
Respiratory system:
Trachea - central
BAE +
NVBS heard
No added
Per abdomen:
Soft, non tender
Bowel sounds - heard
Hernial orifices - normal
No palpable masses
Provisional diagnosis:
Cervical myelopathy?
Potts spine?
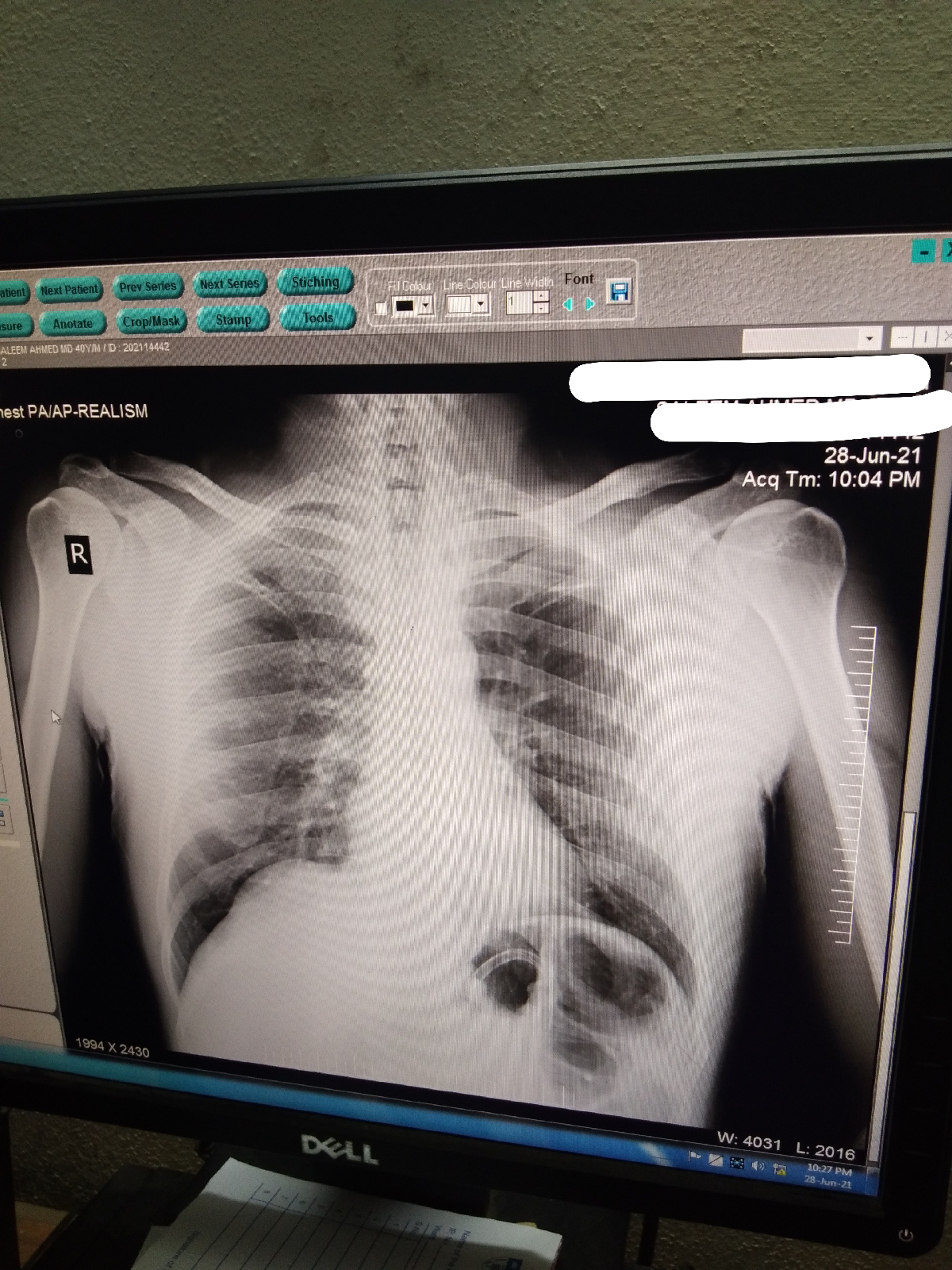
Investigations:
Treatment given:
1. Inj. Optineuron 1Amp in 100ml NS IV/OD
2. Inj. Thiamine 200mg in 100ml NS IV/TID
3. ATT - according to body weight 2 tab PO/OD
4. Bp/ PR/ Spo2/ Temp charting
Update:
FINAL DIAGNOSIS: Quadreparesis secondary to infectious spondylitis of C4, C5, C6, C7 and D1 with Epidural abscess at C5 - C6 level.
Diagnosis:
Quadreparesis secondary to infectious spondylitis of C4, C5, C6, C7 and D1 with Epidural abscess at C5 - C6 level.
Treatment given:
Day 1:
1. Inj. Optineuron 1Amp in 100ml NS IV/OD
2. Inj. Thiamine 200mg in 100ml NS IV/TID
3. ATT - according to body weight 2 tab PO/OD
4. Bp/ PR/ Spo2/ Temp charting
Day 2&3:
Same treatment followed.
Day 4:
Inj. Monocef added.
Advice at Discharge:
Referred to Higher center for neurosurgical decompression as MRI showed
1. Infectious spondylitis of C4, C5, C6, C7 and D1 vertebral bodies with significant erosion at C5 - C6 level and the intervening disc space.
2. Epidural abscess at C5 - C6 level measuring 58 x 4 x 18 mm causing cord compression and posterior displacement of the cord.
3. T2/STIR mild cord hyperintensity - suggestive of edema.
4. Prevertebral collection (max AP dimension - 10 mm) extending from C2 to D3 level suggestive of anterior ligamentous spread.
UPDATE:
He had surgical drainage of abcess at Osmania and getting discharged tomorrow
Outcome of intervention :
Patient regained control over bowel and bladder,
Improvement in power and tone..( as he is walking now)
Adviced to continue ATT.















Comments
Post a Comment