40 year old male with ? acute pancreatitis
This is an online e log book to discuss our patient de-identified health data identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 40 year old male came to the casuality with chief complaints of abdominal pain since morning and vomitings since evening 5pm.
History of present illness:
Patient was apparently asymptomatic 3 years back. Then developed abdominal pain and vomitings and was diagnosed as acute interstitial pancreatitis. For which, he received treatment in the hospital (KIMS) for 1 week.
Patient had similar complaints of abdominal pain, vomitings, constipation 1 year back.
Pain abdomen:
Site - epigastric region,
pricking type, non radiating,
relieved on bending forward position.
H/O vomitings: 10 episodes, non projectile with food particles as content.
CVS, CNS, RS - normal
CT scan: interstitial edematous pancreatitis, no evidence of necrosis, mild ascites, CTSS - 6/10
Again in January, patient came with complaints of pain abdomen (site: umbilical region) radiating to back and was diagnosed as acute on chronic pancreatitis secondary to alcohol consumption.
Now, he came with complaints of pain abdomen since morning, which is squeezing type, non progressive, aggravated on food intake.
H/o vomitings - 5 to 6 episodes since evening 5pm.
C/o decreased urine output
No c/o chest pain, palpitations, syncopal attacks, sob, orthopnea, PND.
Past history:
Not a known case of HTN, DM, CAD, ASTHMA, TB, CVA, Thyroid disorders.
No H/o surgeries and blood transfusions in the past.
Personal history:
He takes mixed diet.
Appetite - normal
Sleep - Adequate
Bowel habits - not passing stools since morning.
Decreased urine output
Addictions:
- Alcoholic since 7 years: consumes 180 - 360 ml/day
Last binge - yesterday
No known drug allergies.
Family history:
No significant family history.
General examination:
Patient is conscious, coherent, co-operative and oriented to time, place and person.
No pallor, icterus, cyanosis, clubbing, koilonychia, generalized lymphadenopathy and edema
Vitals:
Temp - 98.9 °F
PR - 100 BPM
BP - 150/90 mm Hg
RR - 24cpm
GRBS - 124 mg/dl
Systemic examination:
Per abdomen:
Soft
Tenderness + : in epigastric region
No palpable masses
Hernial orifices - normal
Bowel sounds - heard
CVS:
S1, S2 heard
No thrills and Murmurs
Respiratory system:
BAE +
NVBS heard
Trachea - Central
No adventitious sounds
CNS:
Speech - normal
No signs of meningeal irritation
Motor and sensory system - normal
Cranial nerves - intact
Reflexes - present
Provisional diagnosis:
Acute on chronic pancreatitis
Investigations:
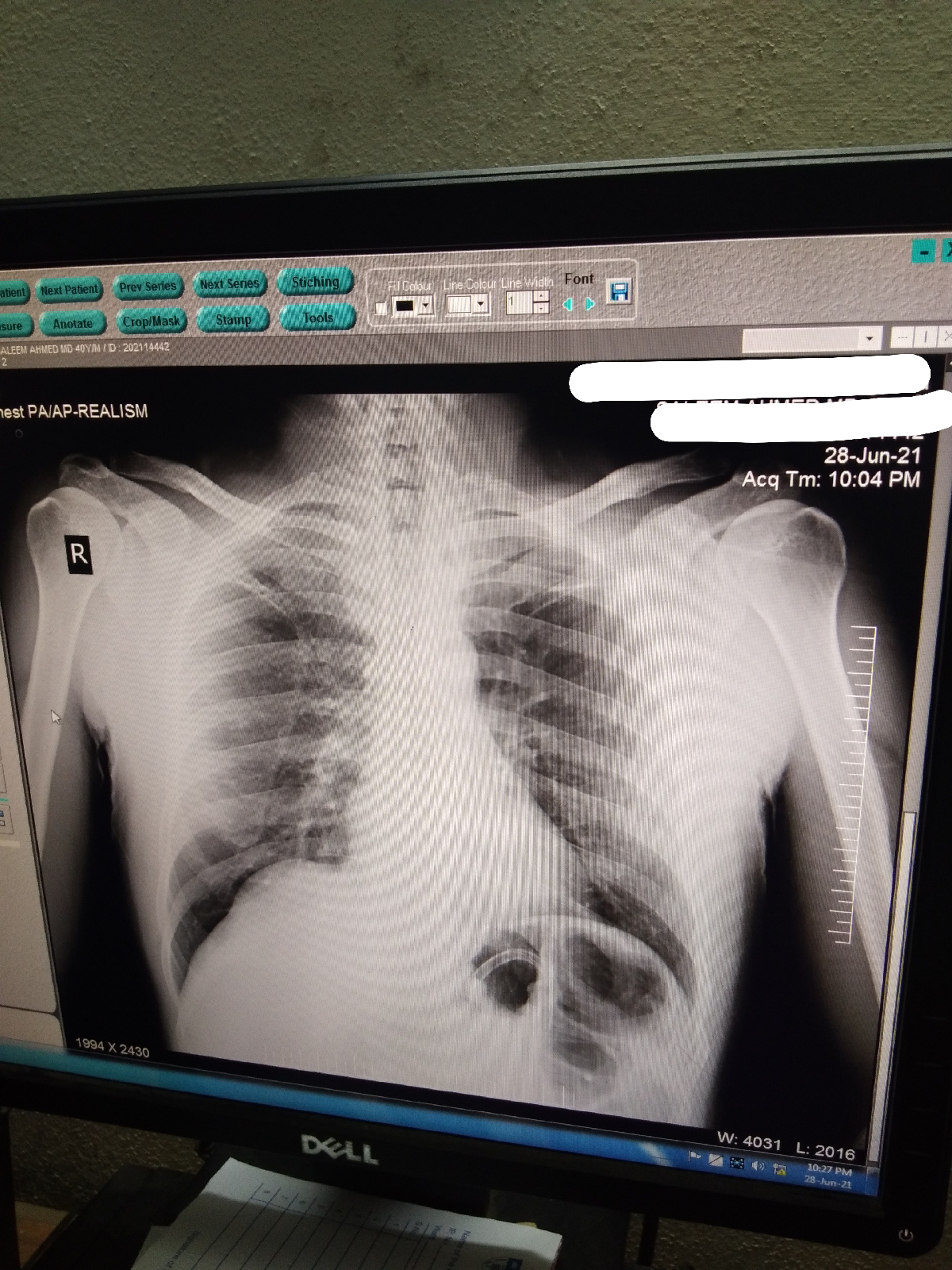
X- ray Erect abdomen:
Treatment given:
1. Nil per oral till further orders.
2. IV fluids - NS & RL @ 125ml/hr
3. Inj. TRAMADOL 50 mg in 100ml NS IV/TID
4. Inj. ZOFER 4mg IV/TID
5. Inj. PAN 40mg IV/OD
6. BP, PR, Temp, RR monitoring 4th hourly
7. Abdominal girth monitoring 2nd hourly



Comments
Post a Comment